Understanding the Genetics of Cancer
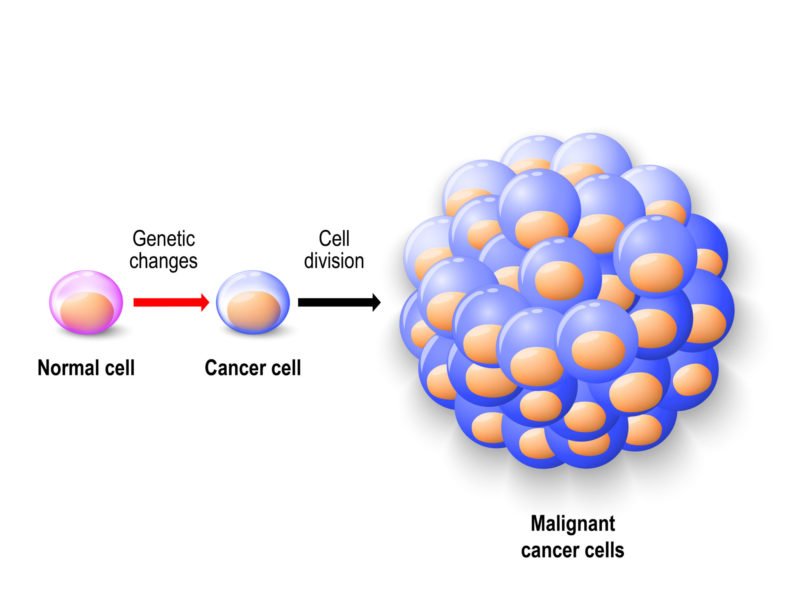
The National Cancer Institute (NCI) defines cancer as the abnormal growth and division of cells (1). Sometimes this is the result of genetic matters and other times it is acquired through the stressors we encounter in our lives. By understanding the genetics of cancer and which gene changes lead to cancer, we can improve detection and practice prevention of cancer.
Which Gene Changes Result in Cancer?
Cancer cells have more mutations than healthy cells. Each person has a different set of genetic mutations and epigenetic modifications. There are multiple gene mutations that our DNA can experience. Nucleotides are the basic structural unit of DNA. Some mutations only impact one nucleotide, meaning one nucleotide is either missing or replaced by another (1). There are also genetic changes referred to as duplications, deletions, and rearrangements that affect long strands of DNA (1). Epigenetic modifications (addition or removal of chemicals in DNA) are not direct changes in DNA itself, but they can still increase cancer risk.
Oncogenes
An oncogene is a “bad” gene that is permanently activated when it is not supposed to be and this causes cells to continuously grow and divide (2). Oncogenes are made through mutations in the normal proto-oncogene cells in our body. When these proto-oncogenes are mutated and become the oncogenes it causes a few cancer syndromes (2).
These oncogenes are normally acquired throughout our lifetime, rather than inherited (2). Oncogenes are normally activated by chromosome rearrangements or gene duplications. Chromosome rearrangements are when one is moved to next to another gene that allows the activation of a gene, and gene duplication possessing extra copies of a gene which can cause overproduction of a protein (2).
Tumor Suppressor Genes
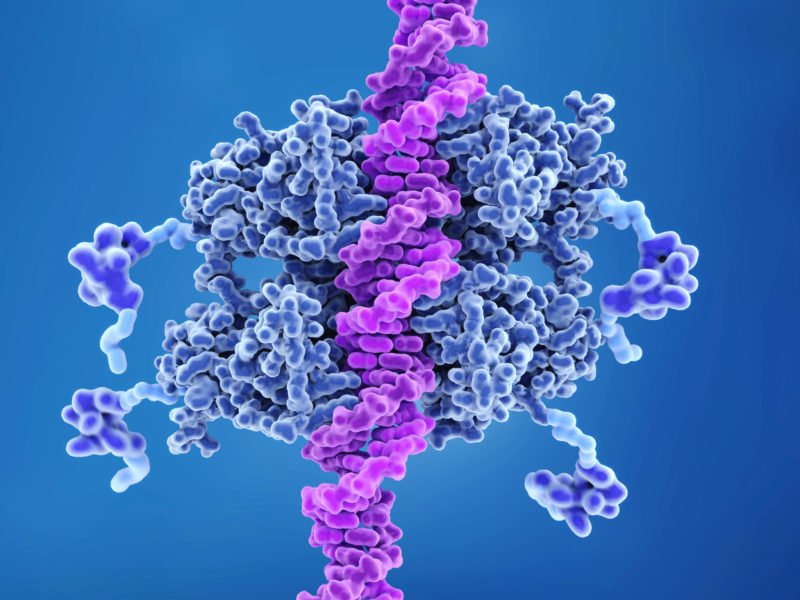
Tumor suppressor genes are genes that slow down cell growth, repair DNA mistakes, or induce apoptosis (programmed cell death) (2). Cancer happens when these tumor suppressor genes do not function correctly. Tumor suppressor genes cause cancer when they’re turned off, while oncogenes cause cancer when they are turned on (2). Mutations in tumor suppressor genes can be inherited, but like mutations in oncogenes, they’re usually acquired.
Is Cancer Genetic?
Cancer is caused by certain gene changes that control the way our cells function, specifically regarding growth and division (1). Genes control the proteins we produce in the body. A disruption in the normal activity of our genes can cause cells to grow and divide irregularly. Cancer occurs when gene changes make a protein that causes cells to grow, or a nonfunctional protein (1).
Hereditary cancer happens when genetic changes are in germ cells (sperm and egg). These germline changes are passed from parent to child and are present in every cell of the child (1).
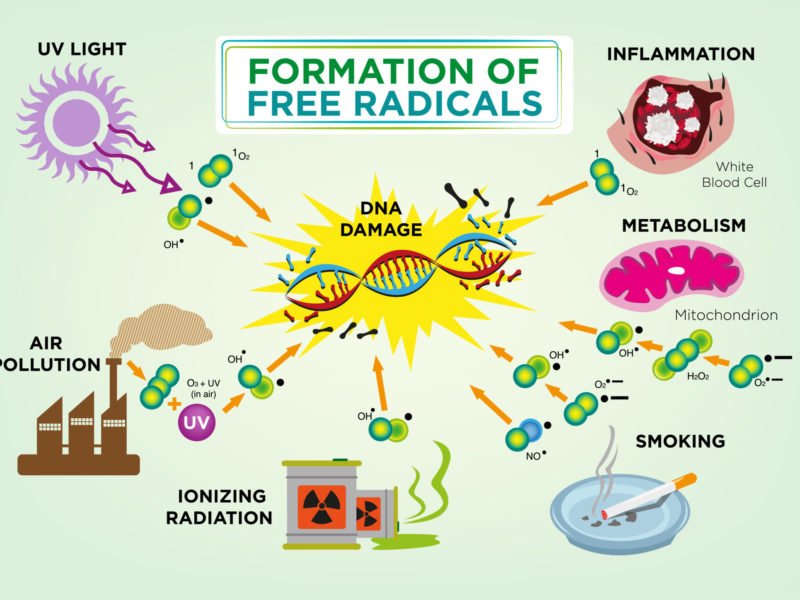
Somatic changes, or genetic changes that occur after conception also cause cancer. Cancer that is caused by acquired mutations is called sporadic cancer. These genetic mutations can occur throughout a lifetime, and they can be a result of cell division errors or exposure to carcinogenic chemicals (1). Carcinogenic chemicals are substances that alter our DNA, for example, tobacco smoke and ultra-violet light greatly impact our DNA (1).
Inherited Cancer Syndromes
Hereditary cancer syndromes are mutations/disorders that may put individuals at a higher risk of developing certain cancers. Inherited genetic mutations are responsible for 5% to 10% of all cancers (1).
Li-Fraumeni Syndrome
A very commonly mutated gene in all cancers is the tP53 gene. The tP53 gene produces a protein that suppresses tumor growth, and when not functioning properly cancer forms. Germline mutations in the tP53 gene can also lead to Li-Fraumeni Syndrome. Li-Fraumeni Syndrome is an inherited disorder that puts someone at a higher risk of developing certain cancers (1).
Lynch Syndrome
Lynch Syndrome is an inherited disorder that increases a person’s risk for certain types of cancers (4). Lynch Syndrome especially increases the risk for colorectal cancer (cancer of the large intestine and rectum) (4). Lynch Syndrome usually occurs when there are mutations in the following genes: MLH1, MSH2, MSH6, PMS2, or EPCAM. These genes function in DNA repair errors, and therefore mutations here result in errors of DNA (4). Lynch Syndrome is inherited through an autosomal dominant pattern, so if an individual has one copy of a mutated gene that is enough to increase cancer risk (4).
BRCA1 and BRCA2 Genes
Other genes linked to hereditary cancer are the BRCA1 and BRCA2 genes. These genes are associated with hereditary breast cancer and ovarian cancer syndrome. Ovarian cancer syndrome means someone has a high risk of developing breast cancer and ovarian cancers throughout their lifetime (1). Other cancer types associated with ovarian cancer syndrome are male breast cancer and prostate cancer (1).
Preventative Measures
There are lifestyle choices you can make to prevent the development of cancer in your body. A few ways to protect yourself from cancer are:
- Avoid tobacco use. Smoking tobacco can lead to lung cancer and colon cancer, as well as many others (throat, bladder, kidney) (6).
- Eat healthy & exercise regularly. Eating healthy and exercising regularly helps keep your body weight low. Eating a proper diet can help prevent against heart disease, and in turn lower risk for prostate cancer. Exercise can reduce a woman’s risk to develop breast and ovarian cancer (6). A low body weight is important because obesity is a risk factor for certain types of cancer.
- Limit alcohol. Alcohol can increase the risk for cancers of the mouth, liver cancer, colon cancer, and breast cancer. If you’re going to drink alcohol it should be in very moderate amounts (1 or 2 drinks per day) (6).
- Avoid exposure to toxic chemicals. This could be environmental (UV light) or industrial (asbestos fibers, benzene, and aromatic amines). UV light can increase the risk of skin cancers, and industrial chemicals are usually full of cancer-causing agents (6).
- Vitamin D consumption. Researchers believe vitamin D supplements may decrease the risk of prostate and colon cancer.
Many of these lifestyle choices also affect your likelihood of developing other common diseases such as heart disease and diabetes. To learn more, read our post about the genetic impacts of a healthy lifestyle.
Genetic Tests for Cancer
If you have a family cancer history, then it’s a good idea to invest in genetic testing for hereditary cancer. Genetic testing for cancer can tell you and your healthcare professional whether you have a specific gene mutation for cancer (for example a mutation in the BRCA1 or BRCA2 gene) (1). Sometimes family members believe there’s hereditary cancer in their family, but the cancer is actually a result of a shared lifestyle (1). This could be the area they live in or the choices they make, such as smoking.
Genetics play a considerable role in the risk assessment for cancer. By having a knowledge of the genetics of cancer and your family history you can make an informed decision about whether or not to undergo genetic counseling. If you do choose genetic counseling as a part of your healthcare plan, a genetic counselor can help you understand your genetic risks (5).
Citations
- https://www.cancer.gov/about-cancer/causes-prevention/genetics
- https://www.cancer.org/cancer/cancer-causes/genetics/genes-and-cancer/oncogenes-tumor-suppressor-genes.html
- https://ghr.nlm.nih.gov/gene/TP53#normalfunction
- https://ghr.nlm.nih.gov/condition/lynch-syndrome#definition
- https://medlineplus.gov/geneticcounseling.html
- https://www.health.harvard.edu/newsletter_article/The-10-commandments-of-cancer-prevention

 Genetic Impacts of a Healthy Lifestyle
Genetic Impacts of a Healthy Lifestyle